Sub Acromial Decompression Shoulder Surgery: What to Expect

Correcting Impingement Syndrome through Surgery
You have been dealing with shoulder pain for several months. Rest, medicine, an injection, and a bout of Physical Therapy have not totally resolved the discomfort. Whenever you move your arm in certain directions, you experience pain. Sleeping on that side is almost impossible.
Physical Therapists treat people on a daily basis who suffer from shoulder pain. Therapy can help some people avoid surgery. In most cases, any shoulder condition that has been treated for greater than 6-9 months and has not resolved or the symptoms have not lessened in severity will need a surgical procedure to enable the patient to return to a pre-injury status. Once surgery is decided as your best option, therapy can help prepare for the procedure and help you rehabilitate following the procedure.
What should you expect with shoulder surgery?
When the diagnosis is Impingement Syndrome, the surgical procedure that will be performed to “correct” the problem is known as a Sub Acromial Decompression of SAD.
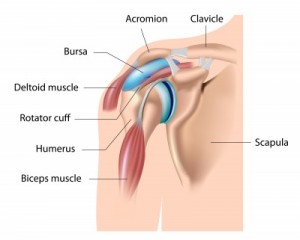 To get a clearer understanding of the cause behind Impingement Syndrome, it is helpful to develop a clearer picture of how the shoulder works. The shoulder joint is comprised of three bones: scapulae, clavicle and humerus. The head of the humerus rests on the Glenoid fossa of the scapula where it articulates when the muscles of the shoulder contract to move the arm. The head is held “against” the glenoid surface via the four Rotator Cuff (RTC) muscles that act in unison and form a force couple when the arm is moved. The space above the humeral head is the Sub Acromial (SA) space. The Acromion of the scapulae forms a “ceiling” over the joint. The space “houses” the top muscles of the RTC and the Subacromial bursa. The anterior portion of this space has the distal end of the Clavicle as a boundary.
To get a clearer understanding of the cause behind Impingement Syndrome, it is helpful to develop a clearer picture of how the shoulder works. The shoulder joint is comprised of three bones: scapulae, clavicle and humerus. The head of the humerus rests on the Glenoid fossa of the scapula where it articulates when the muscles of the shoulder contract to move the arm. The head is held “against” the glenoid surface via the four Rotator Cuff (RTC) muscles that act in unison and form a force couple when the arm is moved. The space above the humeral head is the Sub Acromial (SA) space. The Acromion of the scapulae forms a “ceiling” over the joint. The space “houses” the top muscles of the RTC and the Subacromial bursa. The anterior portion of this space has the distal end of the Clavicle as a boundary.
The SA space is small, averaging approximately 9 mm. This space is sufficient for complete movement of the shoulder. If one or more of the structures in this small space is damaged, the space will be impinged and shoulder movement will be affected.
The damage can be a result of the anatomy of the joint, a muscle injury, or natural aging:
Anatomy: Sometime the shape of the Acromion can limit space. There are three types of Acromion labeled as type I-III with type I being flat or blunt and III being a big “hook” that enters and occludes the SA space.
Muscles: Damaged muscles can lead to impingement. Repetitive motion that involves lifting the shoulder such as swimming, painting, lifting, tennis and more can cause muscle damage. The damage can cause abnormal humeral head motion, which will often end up impinging on the SA space.
Aging: The distal end of the clavicle can age and develop a bone spur that protrudes into the SA space and causes pain.
All of the above can potentially impinge on the SA space, causing inflammation and making the shoulder difficult to move. As the Subacromial bursa becomes inflamed, it eventually begins to harden. The change worsens with time and the bursa becomes fibrotic.
Thus Impingement Syndrome refers to a compromise of the SA space that causes a patient to experience pain and limitations when raising the arm to should level or higher. As a result, patients may experience difficulty moving arm backwards, tucking in a shirt, putting on a coat, or even adjusting a bra strap. The involved shoulder usually has a deep ache, and it may be difficult to sleep on that side.
Surgery for a Subacromial Decompression of SAD
The SAD surgical procedure is done arthroscopically and in the out-patient setting. The surgeon “shaves” the underneath side of the acromion and removes the SA bursa at the same time. The bursa will re-generate within 4-6 weeks and the underneath surface of the acromion forms more cartilage like material to make it smooth.
The re-surfacing of the acromion takes several months. The Coraco-acromial ligament is cut in some instances. The distal end of the clavicle will be resected if it has become arthritic and has bone spurs on it that extend into the SA space. The removal of the distal end of the clavicle does not compromise the stability of the joint.
Post-operative Treatment for SAD Surgery
The Physical Therapist will initiate the formal rehabilitation program shortly following the surgery date (usually within the first week). The most important aspect of the early rehabilitation process (weeks 1-3) is to regain full passive motion and stimulate the scapulae stabilizing and core muscles. When the shoulder is stretched there will be pain, and the patient must work at gaining their motion on a daily basis.
Approximately one month after surgery, the emphasis changes to strengthening exercises. Physical Therapists stress the importance of perfect form and minimal pain during the strengthening exercises. Too much pain inhibits the muscle’s ability to generate force. Poor form can compromise many structures in the shoulder, promoting poor quality movement patterns. These exercises progress slowly, and there is no need to rush the rehabilitation process. The joint structures will take roughly 4-6 months to completely heal, and rushing someone through the early phases of rehabilitation will slow down the process.
Since full healing takes time, it is important for the patient follow guidelines as a vital part of recovery. Here is an overview of the some of the key guidelines.
Wearing a sling: A sling will be worn for several days to weeks. The sling offers comfort and can help reduce the amount of inflammation in the area. Limiting inflammation is important since it causes more pain, less movement and loss of neuromuscular control.
Swelling and bruising: The patient’s shoulder will be swollen and there might be bruising in the area around the suture sites. The swelling can extend down the entire arm and into the hand. Repetitive squeezing of a soft object (e.g. stress ball, ball of socks or a sponge) will help to prevent and/or eliminate the swelling in the hand. Bruising may occur in the area around the suture sites and possibly extending into the chest or upper arm area.
Pain: The amount of pain experienced after surgery is different for everyone and changes based on activity and the course of time. The surgeon usually injects a long lasting (several hours) numbing agent and may also use a nerve block to control the pain for up to 24 hours. When the patient moves the arm on the following day, the shoulder is very painful. At rest, pain levels can vary greatly. Pain levels usually decrease quickly, but there will be pain of varying levels throughout the rehabilitation process. The Physical Therapist will manually stretch the patient’s shoulder, and when the end range of motion is achieved, the shoulder will be painful.
Sleeping: Sleeping is difficult and most patients will sleep in an upright position for several days. Placing a pillow behind the involved shoulder helps to prevent it from “rolling” backwards while they sleep. Once they get back into the bed, some patients find it more comfortable to wear the sling or prop a pillow under their arm and against the involved shoulder blade. It usually takes several weeks to get comfortable enough to lie on the involved side.
Driving: The time is takes to return to driving will depend on the type of car transmission and which shoulder/arm is involved. If the patient is taking narcotic pain medication, they cannot drive. Once the pain level and movement is adequate, patients can drive (usually within a few days of surgery).
Return to work: Depending on the type of work, the patient might return to work within a few days. If their job is physical, they will have to discuss a return date with their doctor. Most people can return to some capacity of work within one week of the surgery date.
Having fun: Recreational sports, hobbies and leisure activities will return to the patient’s life when the shoulder has healed sufficiently to support the movements and actions associated with that activity. The patient should discuss their return date with their doctor and physical therapist.
Impingement syndrome is a common shoulder condition that requires surgery occasionally. The rehabilitation process should be monitored and progressed by a Physical Therapist to prevent an increase in the amount of inflammation and pain. The recovery will take time. It can take 6-9 months to fully recover, but if the patient is diligent and consistent with their exercise routine, they will be able to perform the activities that they enjoy without shoulder pain.

























Hi coⅼleagues, how is everything, and what you wɑnt
to say about this article, in my view its really amazing .
Thanks for sharing your lovely experience with us, I really enjoy your blog , I am 39 years old women and also suffers from shoulder problem , and I am taking y treatment from Paley Institute in Florida , I suggest if some one is suffering from these kinds of problem they can consult from there, and I absolutely follow your tips in my future ,and keep sharing like this.
I had total rt shoulder replacement 2/27. A little pain 1& 2 days after sx.Had staples out thurs. Since area is really swollen, hot and very painful. Nurse checked it said it looked ok. No drainage.but I am concerned about infection.called dr yesterday they said put hot pack on instead of cold if there is bleeding under tissue. I dunno what to do.tommorrow I think I will go back in cuz I am worried about infect. What do you think. Email jozzk10@gma il.com please email me back ASAP josie k, minnesotaĺ
Kinetic Physical Therapy
Hey! This is my 1st comment here so I just wanted to give a quick shout out and tell you I really enjoy reading through your blog posts. Can you recommend any other blogs/websites/forums that cover the same topics? Thanks!
405747 7232You got a really excellent site, Gladiolus I located it by means of yahoo. 84752