Rotator Cuff Surgery

Tips For Rotator Cuff Injuries
- Always seek the advice of a Physical Therapist if your shoulder pain has affected your life style. Not all painful shoulders need to have surgery.
- Pre-surgery rehabilitation can shorten post surgical rehabilitation time periods.
- Use ice on your painful shoulder and “actively” rest it. If the pain does not resolve with this approach, seek medical advice from your Therapist or Doctor.
- Sleep with a pillow propped behind your shoulder to prevent it from moving backwards.
- DO NOT actively move your surgically corrected arm before the doctor and therapist tell you it is ok.
Recovering from a Rotator Cuff Injury
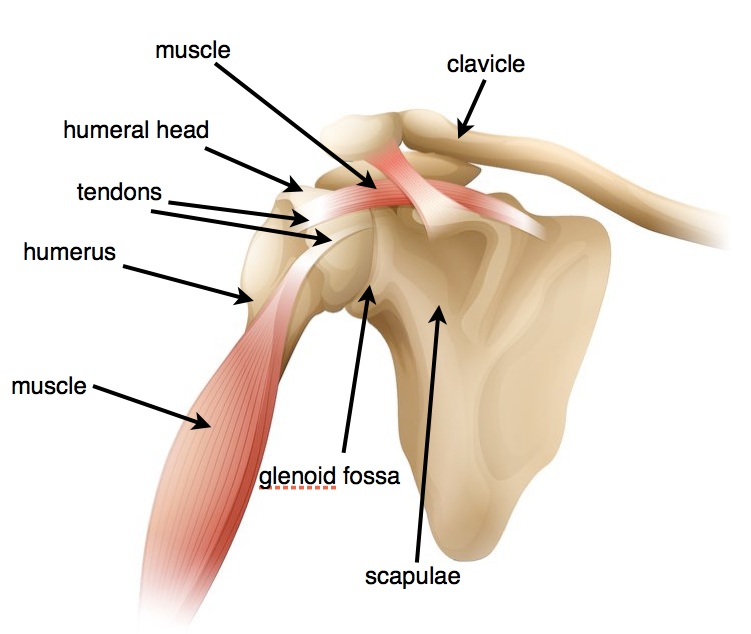
A Rotator Cuff tear is one of the most debilitating injuries to the shoulder. The Rotator Cuff is a group of muscles and tendons that connect the shoulder blade (scapula) to the upper arm (humerus), forming a cuff around the humerus. These muscles and tendons provide dynamic stability to the shoulder joint, allowing the shoulder joint to be the most mobile joint in the body. It can move through every plane of motion, which makes our numerous and various functional activities possible.
This wide range of motion with limited stability also makes the shoulder joint susceptible to injury. As a result, the shoulder joint is commonly injured. Trauma, over exertion, or the natural aging process can cause anyone to suffer an Rotator Cuff injury. If the Rotator Cuff tears, the shoulder joint movement is compromised and becomes abnormal. The result is pain, loss of motion and weakness in the shoulder joint. Over time, these symptoms become worse, indicating a need for surgical repair.
The Rotator Cuff and the Shoulder Joint
Three bones intersect to form the shoulder joint: the scapulae (shoulder blade), the humerus (upper arm), and the clavicle (collarbone). The Rotator Cuff includes four muscles and tendons that connect the humerus to the scapulae. More specifically, the Rotator Cuff muscles are responsible for keeping the humeral head on the glenoid fossa of the scapulae. The movement of the shoulder joint is dependent upon the humeral head’s articulation on this surface.
If the motion is “pure” and normal, the head is held in the center of the fossa by the synchronized muscle action of the Rotator Cuff. Injury to one or more of the muscles affects the synchronized motion and the humeral head moves excessively or abnormally on the fossa’s surface. The Rotator Cuff damage usually occurs at the junction of the muscle tissue and tendon (musculo-tendinous junction), or the tendon tears away from the bone. A full-thickness tear of the Rotator Cuff will not heal on its own and will need to be surgically re-attached to the humeral head.
Rotator Cuff Surgery
Rotator Cuff repairs are done arthroscopically or “open.” The severity and location of the tear will impact how the surgeon determines the approach to use. The most common muscle(s) damage occurs at the top of the Rotator Cuff.
The surgeon repairs the torn tendon, requiring the placement of an “anchor” into the humeral head. This anchor has “barbs” and once put in to the bone it will not “pull” out unless there is a forceful “tug” on it. The anchor has sutures that are threaded through the torn tendon and the tendon is “sewn” back to the bone. The surgeon usually performs a Sub-Acromial Decompression, also. The surgeon protects the repaired tendon by shaving off the underneath side of the Acromion, removing the Sub-acromial bursa and possibly shaving the distal end of the clavicle. Sub-Acromial Decompression makes the sub acromial space larger and gives the repair site more room to prevent excessive compressive forces when the shoulder is moved in certain directions. The bursa will re-generate in a few weeks and shaved bone will be “polished” with new cartilage cells over the course of 4-6 months.
Post Rotator Cuff Repair Recovery
Total recovery takes time and requires protection for the repaired tendon. This includes limited movement for at least 6-8 weeks post op. The patient must avoid active motion as well as excessive passive stretching of the repaired tendon. The surgeon will provide the specifics of the rehabilitation protocols based on the actual surgical procedure performed on the patient and the severity of the damaged tendon(s).
The patient can expect the following as part of recovery:
Pain: The pain tolerance of patients differs greatly, but RCR surgeries are generally painful. The most intense pain is felt within the first two weeks of the surgery. Medication and ice are helpful ways to manage pain. Additionally, the patient can try gentle motion, gentle mobilization techniques, and exercise appropriate for the acute post op phase of healing to help reduce pain.
During the early phase, there is considerable swelling and inflammation throughout the joint. There might be bleeding from the suture sites, but this should be minimal. Bruising might occur in the area of the surgery and extend into the upper arm and chest area.
Wearing a sling: The patient will wake up from the anesthesia with a sling on the involved shoulder. Slings may vary in design based on the specific patient’s needs, but each sling should reduce the strain on the repaired tendon, prevent active motion in the shoulder, and provide comfort to the patient. Some slings will have a “pillow” attached designed to keep the arm in slight abduction, decreasing the tension on the repair site. Most slings will have a waist belt that keeps the arm from being lifted away from the torso. The surgeon will determine the type of sling required and the length of use, but normally the sling is worn at all times and for about 6-8 weeks after surgery.
Motion: NO ACTIVE MOTION involving the repaired tendon for up to 8 weeks. The surgeon determines when the repaired tendon is healed adequately to handle the stress and strain of active motion. The surgeon bases the decision on the quality of the tendon tissue, quality of the repair, size of the repair and other medical conditions that the patient might have.
Sleep: Sleeping is extremely difficult for most RCR patients. It is difficult to get comfortable and to stay asleep. As a result, patients usually spend a couple of weeks leaning back in a recliner chair or sitting up in bed. Patients wear the sling and put pillows behind their involved shoulder to keep it from “rolling” backwards as they sleep.
Once the pain subsides enough for the patients to lie down, they usually lie on their back with the pillow behind their involved shoulder and the sling in place. Rolling onto the un-involved side and “hugging” a pillow with the involved arm is usually comfortable and safe. Lying on the involved side usually does not occur for several months post op.
Driving: The doctor determines when the patient is ready to drive. This usually depends on which arm is involved and in the sling. Additionally, the patient must not take narcotic pain medication when driving. If the right shoulder is recovering from surgery, the doctor may require the patient to wait up to 8 weeks before actively using the shoulder in actions like a stick shift. Patients with an automatic transmission car can usually begin driving sooner. If the patient feels comfortable driving with one arm and the involved arm grasping the steering wheel at the “6 o’clock” position, then they can usually begin driving within the first 2-3 weeks.
Returning to work: The physical requirements of the job will determine how quickly a patient can return to work and in what capacity. Most people can return to some aspect of their job within the first two weeks of the post op time period. Discuss the return date with the surgeon and Physical Therapist.
Having fun: Returning to hobbies, recreational sports and all leisure activities will be determined by the doctor and physical therapist. For more physically demanding activities, it may take up take between 6-12 months for recovery. The repair must heal and the strength must be developed to handle the demands of the activity.
Physical Therapy for Rehabilitation
Physical Therapy is a major aspect of the rehabilitation process. Working with the doctor and patient, the Physical Therapist will design a rehabilitation program specific to the patient.
Initial phase (loosening): Within a few days of surgery, the patient begins therapy to help restore passive motion and reduce swelling, inflammation and pain. This may last up to 8 weeks depending on the surgeon. The therapist emphasizes the scapulae stabilizing muscles and core musculature. He or she will manually stretch the patient’s shoulder joint, which will be painful. The patient must tolerate this pain to avoid having the joint “stiffen” and lose range of motion.
Musculature that is not involved in the surgical repair can be used actively. The patient can resume cardio-vascular exercises that do not jeopardize the repair (e.g. stationary bike and elliptical machine without arm motion, and walking on a treadmill) as soon as they have the desire to perform the activity.
Second phase (strengthening): The second phase of the rehabilitation process incorporates strengthening exercises. At about the 8th week post-op, the patient can begin strengthening exercises. Progress depends upon the patient’s response and usually takes months to complete. Patients commonly take approximately 1 year or more to return normal, pre-injury/surgery status.
Your physical therapist can guide your program and progress it accordingly. The therapist will make sure that the program incorporates core strengthening and a numerous types of exercises for the shoulder, including open and closed chain, dumbbell, sport cord (large rubber bands), and machine exercises.
Rotator Cuff Surgery is used to re-establish the normal function of a shoulder joint that has suffered damage to one or more of the Rotator Cuff tendons. The surgery and rehabilitation are painful at times and take months to return to the pre-injury condition. A comprehensive rehabilitation designed by a well-trained Physical Therapist can restore the normal function of the joint and enable the patient to return to their desired activities.

























I really liked this post and the different phases for PT. I think it is so important for patients and therapists to understand the different phases of recovery. Like mentioned in the article the first phase is about protection and loosening the shoulder joint. This includes immobilization and passive range of motion to try and avoid excessive scar tissue formation. One thing therapists can do during this first phase is take the opportunity to educate patients not only about using slings or pillows to help protect the shoulder but importance of complying with physician precautions and rehabilitation protocol.
Once into the second or strengthening phase it is important for therapists not only to emphasize good strengthening program but address postural awareness or and correct body mechanics for functional activities to avoid further damage or complications. It is the role of the therapists not only to help promote the rehabilitation process but take the opportunity to educate the patient on building a healthy lifestyle.
“Pre-surgery rehabilitation can shorten post surgical rehabilitation time periods.” Great advice … wish my surgeon had emphasized this more!
good
good
good