Multidirectional Instability of the Shoulder

Tid Bits of Info
- If your shoulder “pops-out” one time, it will most likely be fine and “normal” following a prolonged period of rest, protection and rehabilitation.
- If your shoulder “pops-out” 2 or more times there is a good possibility that it will require surgery to fully stabilize it.
- Most dislocations occur when the bone arm bone moves out of the joint in an anterior (front) direction.
- If your shoulder “pops-out” attempt to secure it to your torso and have a skilled healthcare professional help to reduce or re-locate it into the joint.
- Follow the advice of your Physical Therapist and you will have a successful return to your pre-injury status.
The most commonly dislocated joint in the body is the shoulder, and many people suffer from a dislocated shoulder joint at some point. Normally the shoulder will recover after a couple of weeks/months of rest and rehabilitation. If dislocation happens more than once, it will be painful and could limit the full range of movement in the arm. Some people may experience pain or a feeling that the shoulder is about to pop out of joint when moving the arm too high or in certain positions. The joint may require surgery to correct what is known as multi-directional instability.
What is Multidirectional instability?
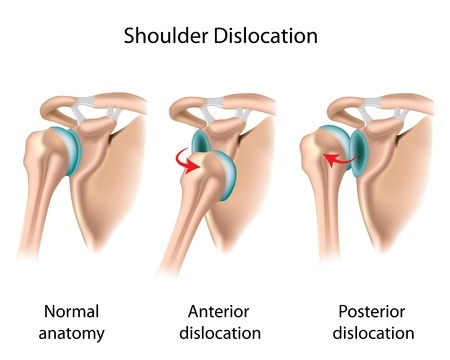
Multidirectional instability (MDI) is a problem in the shoulder joint resulting in ongoing instability in multiple directions. When the shoulder “dislocates,” the humeral head slides out of joint and off of the surface of the Glenoid Fossa and usually moves excessively in an anterior (front of the body) direction.
The humeral head “exits” the joint with great speed and force. After repeated injuries, the anterior capsule, ligaments and labrum, may suffer sustained damaged. As a result, the static stabilizing structures of the anterior aspect of the joint may be damaged to a point of no return.
Damage and Repair of MDI
The labrum is a fibrocartilage disc that deepens the Glenoid Fossa and creates a socket that houses the humeral head more securely. When it is damaged and disconnects from the bony edge of the Glenoid Fossa, it cannot heal on its own. The buttressing capability of the labrum for the humeral head is lost and the head is free to slide forward and out of the joint. If the slippage occurs numerous times, the labrum can be damaged further and the other static stabilizing structures (ligaments and capsule) can be stretched to a length that renders them useless and incapable of providing a stabilizing force.
The labrum can be repaired surgically, and the shoulder joint can regain. If you suffer from the condition of multi-directional instability a surgeon can surgically repair the Labrum via arthroscopy or through an incision, referred to as an “open” procedure. The bone is specially prepared and the surgeon uses “anchors” which have sutures attached to them to hold the torn Labrum to the bone. Over the course of 10-12 weeks, the Labrum re-attaches itself by “growing” fibers that imbed themselves into the bone. At this point in time, the sutures become non-functional and the “live” tissue anchors the Labrum to the bone, enabling the patient to recover and begin their return to full activity level.
Post Surgery Physical Therapy
Physical Therapy can begin shortly following the surgery. The surgeon will restrict certain motions (rotations) to prevent excessive sheer or compressive force being placed across the repaired Labrum. The restrictions will be in place for several weeks/months until the Labrum has adequately re-attached itself to the bone. Initially, the Physical Therapist will seek to control pain and maintain a limited amount of passive motion.
Your Physical Therapist will help you maintain your motion (respecting the surgical restrictions) and begin re-establishing the normal neuromuscular activity of shoulder joint. As the Labrum heals, the goals change to restore strength, motion and function of the involved shoulder.
What to Expect
Pain: Each person experiences pain differently, and post-operative pain will vary from patient to patient. The surgeon usually injects a numbing agent that should last for several hours. A nerve block may also be used to controls the pain for up to 24 hours. The shoulder is very painful the next day when the patient moves the arm. Pain levels at rest can vary greatly and the intense pain usually decreases within a few days. The patient should be prepared to experience varying levels of pain throughout the rehabilitation process. The patient’s shoulder will be manually stretched and mobilized by the therapist, and there will be pain at the end range of motion.
You must communicate with the Physical Therapist when you are being mobilized and inform the therapist of any painful sensations when the movement is in the direction of the surgically restricted motions. These limits need to be protected for the first 6-8 weeks following the surgery.
Wearing a sling: In order to protect the repaired Labrum from quick and sudden motions, the surgeon will require the use of a sling for a couple of weeks. The sling should increase your comfort and reduce the amount of inflammation in the area. The inflammation causes more pain, less movement and loss of neuromuscular control. The surgeon will determine how long a sling should be worn, but it would not be unusual to be in the sling for 6-8 weeks (except during Physical Therapy or performing home exercises).
Swelling and bruising: Your shoulder might be swollen and there might be bruising in the area around the suture sites. The swelling can extend down the entire arm and into the hand. Repetitive squeezing of a soft object (e.g. stress ball, ball of socks or a sponge) will help to prevent and/or eliminate the swelling in the hand. Bruising may occur in the area around the suture sites and possibly extending into the chest or upper arm area. Repetitively bending and straightening of the elbow can help to reduce the swelling and discomfort in the upper arm. When moving the elbow, there should be no weight in the involved hand and the use of the non-involved hand might be needed to help with the motion.
Sleeping: Sleeping is difficult and most patients will sleep in an upright position for several days. The surgeon will require the use of a sling during sleep for several weeks following the surgery. Placing a pillow behind the involved shoulder helps to prevent it from “rolling” backwards while sleeping. When in bed, some patients find it more comfortable to prop a pillow under the arm and against the involved shoulder blade. It usually takes several weeks/months to get comfortable enough to lie on the involved side.
Driving: Returning to the driver’s seat is determined in part by which shoulder is involved, if the transmission is automatic, and if the patient has quit taking narcotics. The doctor ultimately determines when you are ready to drive. Normally, you should be able to resume driving within the three to four weeks following the surgery.
Return to work: Depending on the type of work, you could return to work within a few days. If your job is physical, you’ll have to discuss a return date with their doctor. Most people can return to some capacity of work within one week of the surgery date. If your job is physical in nature, it might be several months before you can return to a full duty capacity. Any job that requires movement of the involved arm above shoulder level will take a minimum of 3 months to be able to return to full duty tasks.
Having fun: The patient can participate in recreational sports, hobbies and leisure activities when the shoulder has healed sufficiently to support the movements and actions associated with that activity. If the activity requires you to throw or move the involved arm above shoulder level repetitively, it will take 4-6 months (minimum!) to begin to prepare the shoulder for a successful return to that activity. You should discuss return date with your doctor and physical therapist.
Multidirectional instability of the shoulder is troublesome, painful and difficult to treat or manage. At times the instability is great enough and the shoulder requires a surgical procedure to re-establish the “normal” anatomy and congruency of the involved bones. Prior to surgery the patient’s shoulder gradually loses the ability to remain fully functional and they will have to modify many of their motions to protect the shoulder from “sliding out”. The patient should expect to return to all pre-injury activities successfully following a surgical repair of the torn Labrum providing they follow the guidelines of the rehabilitation program that will be established by the surgeon and Physical Therapist. The exception to this is a very high level throwing athlete, but even some of those people have beat the odds and returned to their previous skill level.

























