ARE “KNOCKED KNEES” A PROBLEM?

Tid Bits of Info
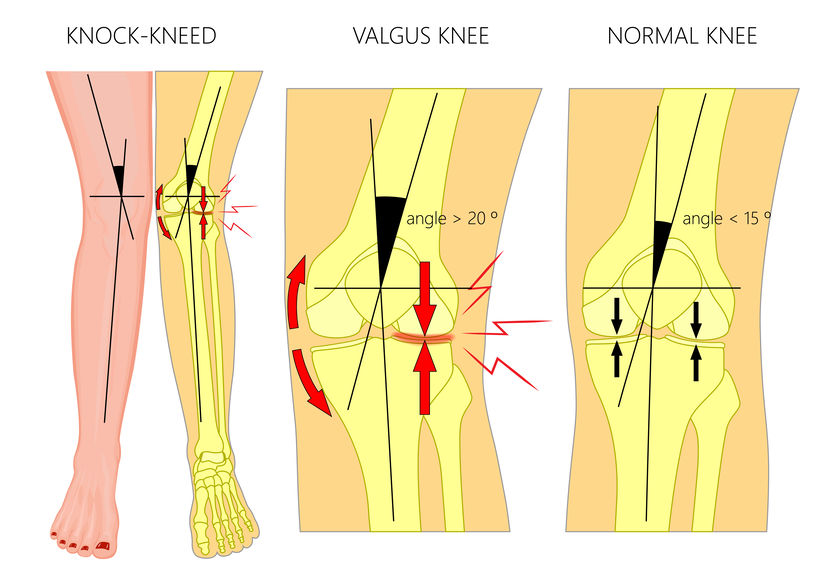
- Genu valgum is the same as “knocked knees.”
- Severe genu valgum or “knocked knees” can lead to osteoarthritis of the lateral side of the joint.
- Severe genu valgum can be surgically corrected by performing a surgical procedure known as an osteotomy.
- “Knocked knees” posture can lead to over-use ankle injuries.
- Seek treatment from a Physical Therapist if you have “knocked knees” and you want to live an active lifestyle.
Most of us are familiar with the term knocked knees and have even used it to describe the shape of knees that move inward and touch. Knocked knees (known as knee valgus or valgus alignment) simply means abnormal knee alignment when two knees are touching each other in a “v” shape. Some children grow out of knocked knees as they age, but adults can also exhibit this condition. What causes knocked knees? Do they pose a risk for injuries? Can you change this condition?
Many healthcare professionals believe that knocked knees place the individual at greater risk of many lower extremity conditions if it is excessive or uncontrolled. Left uncontrolled, dynamic knee valgus can lead to major over-use injuries or a more severe injury to the ligaments of the knee. This alignment of the knees places the medial aspect (closest to the midline of the body) of both knees close together. The appearance of each leg is that of a “v” shape. This alignment can place damaging forces directly or indirectly on the lumbar spine, hips, knees, and the ankle/foot complex. Some believe that it is a “normal” motion but if it is uncontrolled and occurs at a high rate of speed which becomes excessive the forces are too great and an injury will occur.
When treating knee valgus, healthcare professionals seek to assess the movement in the same side (ipsilateral) hip by looking at the amount of valgus that occurs as someone “plants” their foot on the ipsilateral knee. The amount of movement, which has been coined pelvic pronation by some researchers, can help to determine if that person is more susceptible to a lower extremity injury.
Many healthcare professionals contend that too much motion in the acetabulum on the head of the femur can cause so much accessory pelvic and low back motion that some of the naturally occurring musculoskeletal tension that helps to add dynamic support to the lower extremity is lost. The loss of this tension places all of the lower extremity at a disadvantage to be able to control the joints of the ipsilateral leg.
Controlling the amount of valgus at the knee can be partially learned with extensive training. Visual cues, biofeedback and numerous exercises that are performed weight bearing and non-weight bearing can be used to educate or re-educate the movement patterns of the lower extremities
Seeking help from a Physical Therapist who specializes in orthopaedic rehabilitation is helpful. These licensed professionals are able to evaluate your movement patterns and assess what type of exercise routine would be most beneficial for you. In most instances, the person who has excessive and uncontrolled valgus motion in their knees has significant weakness in their core and hips. Particularly the hip extensor, external rotators, and abductor musculature must be the focal point of a rehabilitation program. The best way to avoid an injury is to have these muscle groups strong and ready to respond when “called” upon. If these muscles are strong but have not been trained to contract when they need to contract to offer the dynamic support to the joints of the lower extremity there is increased risk of sustaining an injury. A major portion of any rehabilitation program is to educate the nervous system and the anatomical structures that it controls ( a “fine-tuned” system).
Increased valgus positioning of the knees upon landing can lead to an increase incidence of lower extremity injuries. The best way to correct this condition is via a thorough full body rehabilitation program. The stabilization of the lumbar spine and hips through strengthening exercises and neuromuscular retraining is key to a successful rehabilitation program.
























