TIBIAL PLATEAU FRACTURE

Tid Bits of Info
- Greater than 50% of all tibial plateau fractures occur in people 50 years old or older.
- Osteoporosis can be a primary cause for a low energy tibial plateau fracture.
- The tibial plateau has to sustain forces that can be 7x the body weight.
- The patient must remain NOT WEIGHT BEARING until the doctor reads an x-ray that indicates enough bone healing to transition to full weight bearing.
- Seek the advice of an orthopeadic Physical therapist for the proper rehabilitation program.
Recovering from any fractured bone takes time and requires some form of adaptation. Recovering from a tibial plateau fracture (upper shin bone) will impact day-to-day activity for an extended time. The tibial plateau is the one of the biggest bones in the body, is the weight bearing bone in the lower leg, and directly affects the knee joint. The bone fracture also affects the knee joint and surrounding soft tissues (skin, muscle, nerves, blood vessels, and ligaments). A fractured tibial plateau must be diagnosed and treated immediately to prevent future damage to the knee joint.
Commonly known as the shin bone, the tibia is located below or distal to the thigh bone or femur. It forms the bottom portion of the knee joint and bears 100% of the body weight during activity when someone transitions to single leg stance. This weight-bearing force can become 7 times (or more) of a person’s body weight in certain activities.
The plateau is covered with hyaline (articular) cartilage and is subject to these forces. The normal alignment of the human knee is in a slight valgus position. This alone makes the lateral tibial condyle more susceptible to injury. If the alignment of the plateau and the femoral condyles (distal end of the femur and upper part of the knee joint) is not proper the sheer and compressive forces developed with weight bearing activity can lead to “break down” of the cartilage. This can eventually become osteoarthritis.
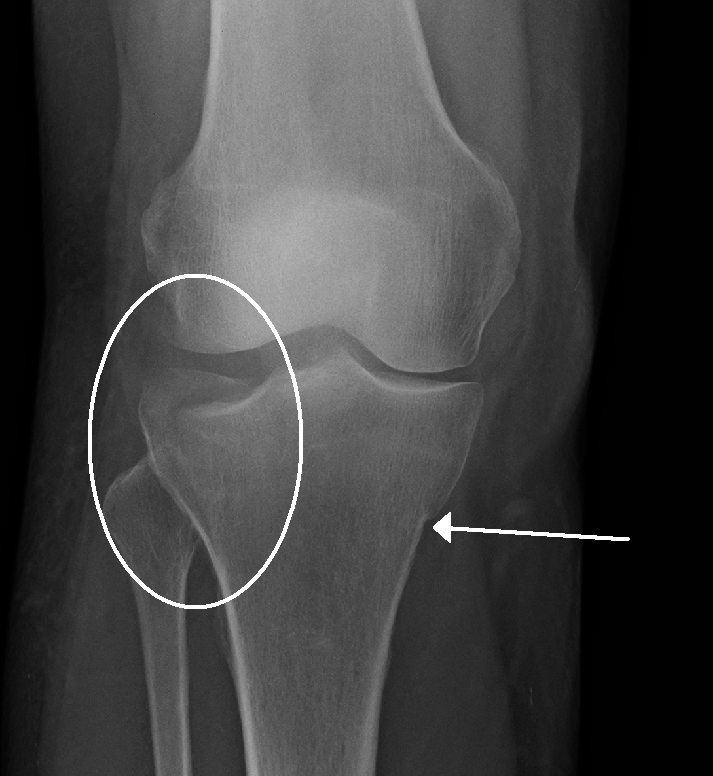
Causes of a Tibial Plateau Fracture
The most common cause of a tibial plateau fracture is a valgus force with axial loading (force pushing outer knee inward). This commonly occurs in auto accidents when the flexed knee makes contact with the dashboard or in sports related injuries when the athlete lands from a jump and the knee “buckles”. At home or at work, people could fall from a height and attempt to land on their feet. While a fracture usually involves a high energy force, minimal or low intensity forces could lead to a fracture for an osteoporotic patient. In the event of a high energy incident the fracture site will most likely be a crack or split in the bone and with low energy incidents the bone is usually crushed.
Over 100 years, medical professionals have developed and modified a classification system for fractures. The idea behind this and any classification system was to be able to “label” a specific fracture in a way that would indicate the type of damage that had occurred when the fracture took place. This could then be used amongst healthcare professionals and be a guide to the treatment protocols.
Today’s classification system includes 6 different classifications of fractures of the tibial plateau. The most commonly used system classifies the fractures by the pattern of the fracture and the fragment anatomy.
- Type I: wedge or split fracture of the lateral condyle with no compression (depressed)
- Type II: wedge or split fracture of the lateral condyle with compression
- Type III: pure compression fracture of the lateral condyle
- Type IV: fracture that involves the medial condyle
- Type V: fracture that involves the both condyles and might include compression on both
- Type VI: complex, bi-condylar fracture with split fragments and compression of both condyles
The treatment of these fractures usually involves a surgical procedure to “fix” the fracture and compression area and a very prolonged period of non-weight bearing (NWB) status. Many of these patients are NWB for 8-12 weeks.
Physical Therapy for a Tibial Plateau Fracture
While physical therapy could begin immediately following the surgical procedure, most patients begin 2-3 weeks after their surgery. It is essential for the patient to remain NWB. Premature “loading” of repaired bone can cause damage and even lead to early onset arthritis of the knee joint. Initial physical therapy treatments target range of motion, pain and swelling reduction and stimulating the neuromuscular activity of all the core and lower extremity musculature.
Core strengthening is imperative during the NWB period. These exercises reduce low back pain that usually develops due to the NWB status and provide the stimulus for the core muscles, which are the foundation to all movement, to be prepared to control the pelvis and lower extremities. When the x-rays indicate that the proper amount of bone healing has occurred, patients will commence upon a full-fledged strengthening program that will enable them to regain full functional capabilities.
Tibial plateau fractures are life changing and need to be properly diagnosed and treated immediately. The damage to the bone can be classified into 1 of 6 categories and following an extensive period of time when the patient will be NWB they will regain full functional capabilities providing they are put through a demanding physical therapy rehabilitation program.

























My surgeon says my bone is not regenerating. Can a bone growth stimulator help? Any other ideas? I am 3 months post op.Help!Thanks.
As a rule, any misalignment from the normal for a particular joint could be compensated by joints above and/ or below the compromised joint. There is a possibility for arthritis to set in it after a while depending on your activity level, your age, the joint affected. LE joints wear weight and are exposed to different angles depending on activity being performed, forces changing constantly in the flow of movement. An experience ortho physician should give you a projection on your particular case.
i just had a 0.6mm depressed lateral TPF surgically repaired a week ago at the recommendation of my orthopedist (stating altered joint dynamics could lead to early arthritis and laxity). not sure if this helps you. good luck.
Thank you, i hope i can recover soon
What is the chance of minimal lateral plateau depression fracture with nonoperative treatment . ???