SHIN SPLINTS

Tid Bits of Info
- Most running shoes should be replaced every 200-250 miles.
- Over the counter orthotics often times are sufficient providing the patient performs specific exercises.
- Walking side-ways with a “rubber band” around your ankles can strengthen the hip musculature sufficiently to eliminate excessive hip motion.
- Some shoes are designed to control excessive pronation.
- Seek the advice of a qualified Physical Therapist for a specific exercise routine that will address the deficiencies that exist throughout the core and lower extremity.
If you experience shin pain after running, dancing, walking or a vigorous-weight bearing exercise, you could be suffering from shin splints or medial tibial stress syndrome. This common pain normally affects the bottom, inside of the part of the shin, but is can also occur in the front of the shin. Shin splints can get very sore to the touch and will hurt when the person walks or runs. Physical Therapists can develop a regimen of exercise to help treat this painful condition.
Shin Splints and the Movement of Foot and Ankle
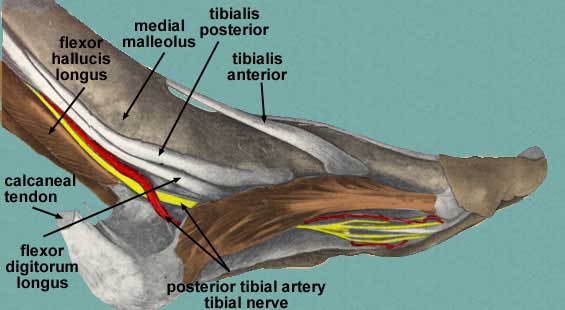
The shin consists of the tibia and fibula and numerous muscles that control the motions of the foot and ankle in the gait cyle (the cycle of motion when walking or running). The gait cycle consists of heel strike, mid-stance and toe off. During the cycle, the arches of the foot move to absorb shock or act as a rigid lever to propel to next step.
The movement in arches is dependent upon shape of the bones, the static stabilizing ligaments and the dynamic stabilizing muscles. The medial longitudinal arch is the part of the foot that can be most affected by weight bearing forces. This arch extends from the heel bone (calcaneus) to the toes on the medial (mid-line) aspect of the foot. The “key stone” of the arch is the navicular bone. This bone has one muscle, the posterior tibialis, that attaches to it and it is controlled by the action of this muscle.
When the arch is “collapsing” and the foot is moving into pronation, the navicular bone is “dropping” down towards the ground. The posterior tibialis muscle contracts eccentrically (elongation of the muscle fibers) and slows down the descent of the navicular bone. Once the medial longitudinal arch collapses to absorb the shock of weight bearing activity, the foot must return to a rigid lever to propel the person forward. The navicular bone is “pulled” upward and away from the ground by the concentrically (shortening of muscle fiber) contracting posterior tibialis muscle. The dual action of the posterior tibialis muscle can have deleterious effects on it when there is too much motion in the arch. When the muscle is “over-worked,” it can become inflamed and cause pain along the shin bone which is the location of its origin.
Causes of Shin Splints
Shin splints can be cause by a variety of factors such as overworking the lower leg, increasing intensity or activity levels, wearing improper shoes, and more. Healthcare professionals evaluate the pain along the medial aspect of the tibia as well as the core and entire leg. The core musculature is the foundation of all lower extremity action therefore it must be well trained and functioning well to be able to control the pelvis. The lower extremity functions as a unit and forms a “kinetic chain”. Starting at the hip, the evaluation must examine the strength of the musculature. If the femur internally rotates excessively upon landing or foot contact with the ground during the gait cycle, it is usually secondary to weakness in the external rotators, extensors, and abducting hip muscles. The excess internal rotation of the femur can force the tibia (shin bond) into an excessive amount of internal rotation as the person moves from heel strike to mid stance in the gait cycle. When the tibia internally rotates too much, it literally forces the talus (ankle) and navicular bone down towards the floor causing excessive pronation or “collapsing” of the medial longitudinal arch and this can cause shin splints.
Wearing shoes that do not support the medial longitudinal arch during the gait cycle can cause a great deal of problems in the foot and shin. The shoe must be able to “control” and offer support to the arch during all kinds of weight bearing activities. The proper shoe will control the amount of motion that occurs in the arch regardless of the amount of weight bearing force that is put through the arch during a given activity. A shoe that does not offer enough support will enable the foot to pronate excessively and place too much stress on the posterior tibialis muscle leading to shin splints. If the shoe is not able to control the foot adequately the clinician might suggest the use of an over the counter or custom semi-rigid or rigid orthotic. This is an insert that replaces the existing insole of the running shoe and the custom device is specifically designed for the individual’s foot. These inserts are hard and made of graphite, polypropylene or other plastic-like materials.
Treating Shin Splints
Initial treatment is the same as any musculoskeletal injury. The RICE principle (Rest, Ice, Compression and Elevation) for acute injures should be followed and it should help control the inflammatory process that is causing the pain. All weight bearing activities might have to be modified. The person suffering from shin splints might benefit from new or different shoes and possibly a pair of custom or “over-the-counter” orthotics. A Physical Therapist can educate you in the proper exercise routine to perform to help to strengthen or stretch all of the involved muscles. If the symptoms do not resolve with the acute treatment, visit the doctor to rule out a stress fracture.
Physical Therapists who work with orthopaedic injuries are the best-qualified healthcare professionals to adequately assess the status of the lower extremity kinetic chain. They are educated to evaluate and develop a treatment protocol that will reduce the stress and strain on the posterior tibialis muscle and help to prevent or treat shin splints. Some are able to cast and fabricate custom orthotics.
Shin splints or medial tibial stress syndrome can affect our ability to perform weight-bearing activities and force us to stop performing certain activities. In most cases, the symptoms can be treated successfully with specific core and lower extremity exercises. Acute orthopaedic injuries may require the use of an orthotic and treatment techniques utilized for acute.