PELVIC FLOOR DYSFUNCTION (PFD)

Tid Bits of Info
- Treatment of PFD can alleviate or eliminate symptoms approximately 75% of the time.
- PFD can affect anyone of any age, gender or race.
- One of three women suffers from PFD.
- Muscles of the pelvic floor are similar to any other muscle and can be strengthened and regain full function.
- Certain Physical Therapists specialize in the treatment of PFD.
Millions of people silently suffer from pelvic floor dysfunction (PFD). Often undiagnosed this painful and embarrassing condition can be treated, and patients usually experience a reduction in symptoms from a range of techniques. If you know someone suffering from ongoing pelvic pain, abdominal pain, tailbone pain, urinary incontinence, and a range of similar symptoms, you might direct them to this blog for helpful information that could address the condition.
What is pelvic floor dysfunction? What is the pelvic floor? Can this condition effect anyone or is related to one sex, age or race? Can it be fixed and does the patient have to have surgery or take medication? These are some of the common questions asked when discussing pelvic floor dysfunction (PFD) with almost anyone. The following paragraphs answer these and other common questions related to PFD.
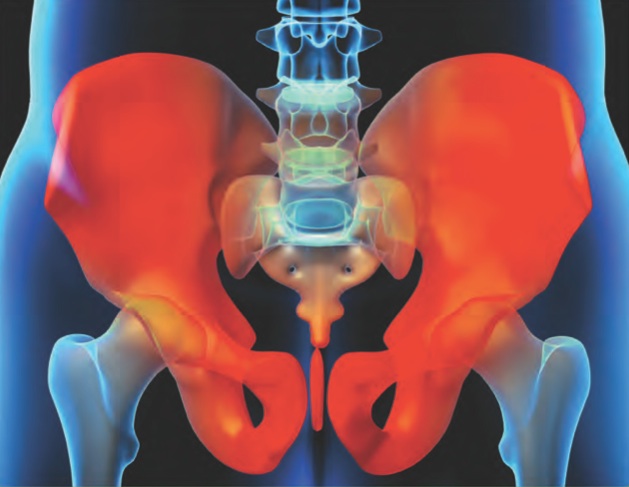
A Quick Overview of Pelvic Floor Dysfunction
The pelvic floor is made of a group muscles, tendons and ligaments that act like a hammock and help to hold the organs: bladder, uterus (women), prostate (men) and rectum (the distal end of the large intestine that stores solid waste). These muscles contract and relax in conjunction with the abdominal muscles to help to control the functions of bowel and bladder. When the coordination between contracting and relaxing does not occur correctly, there is a malfunction in the system and the person will suffer from PFD. The muscles may spasm or can be too weak to perform their function. There can be hypo or hyper-sensitivity to different structures in the pelvic region that leads to the dysfunction.
Causes of Pelvic Floor Dysfunction
The cause of PFD is often times not known. Any number of causes have been noted during a lengthy and detailed interview process at the time of an evaluation. Traumatic injuries, vaginal childbirth, infections, pregnancy, poor posture, chronic low back and SI joint pain, systemic neuromuscular diseases and insidious onset are some of the suspected causes that have been discussed by some patients.
Conditions/Symptoms of Pelvic Floor Dysfunction
There are many symptoms that are associated with PFD. If you are suffering from any of the following, seek medical help.
- Pelvic pain
- Constant or chronic constipation
- Painful intercourse
- Incontinence
- Urinary urge or painful urination
- Feeling of incomplete bowel movement or the need for several bowel movements
- Low back pain of unknown origin
- Urine or fecal leakage
- Abdominal pain
- Pregnancy and postpartum conditions
- Coccydynia (Tailbone pain)
- Gynecological cancer (Pre and post chemo therapy)
- Pudendal Neuralgia
- Athletic injuries
- Menopausal symptoms
- Endometriosis
- Vulvodynia
- Interstitial cysitits (painful Bladder syndrome)
- Irritable Bowel Syndrome
Diagnosing Pelvic Floor Dysfunction
Details of Condition: The healthcare professional will take an extensive history when you visit, including location and intensity of pain and all aspects of your pelvis. The types of questions will include the following: When do you have pain and what can you do to relieve it. Do you have pain during intercourse? Do you have chronic episodes of constipation, urinary incontinence or urine or fecal leakage? Do you urinate more frequently than every 2 hours? Does your back, hips or abdomen hurt? Have you given birth vaginally? Basically, the healthcare professional will need to gather information that deals with all aspects of your pelvis.
Assessment: The healthcare professional will then perform an external (possibly with surface electrodes that record muscle activity) and internal (manual) examination the muscles of the pelvic floor. The evaluation will include an assessment of the activity and strength the muscles. Special techniques enable the professional to assess the quality of contraction and the force that the muscles are able to generate.
If chronic constipation is the primary problem, a defecating proctogram can be performed. This is done with dye and a video of the movement of the dye and pelvic floor musculature and rectum activity as the person attempts to empty the dye colored fluid out of the rectum.
Treatment for Pelvic Floor Dysfunction
Physical Therapists utilize a range of specialized techniques and training to treat PFD. Approximately 75% of all patients respond favorably and experience a significant reduction in their symptoms (many have total resolution). These techniques are painless and can include biofeedback which can be in several different forms. The therapist might use video or sensors that emit a signal when the pelvic floor muscle is active. This helps to teach the patient what the proper sensation should be when everything is “working correctly.” The therapist can utilize manual stimulation, massage or stretches that help to alleviate symptoms of tight or weak muscles.
Physical Therapists teach patients relaxation techniques and targeted strengthening exercises. There is even specialized equipment that can help to build strength and endurance of the involved muscles.
The patient might be placed on certain medicines to help combat the symptoms and in the worst case scenario surgery might be needed to eliminate the problems.
Pelvic Floor Dysfunction is extremely common in our society and it can affect anyone. PFD has been a condition that many people have chosen to live with because of embarrassment or simply no one could help them resolve their symptoms. Physical Therapists are able to help almost everyone with PFD. Seek medical attention if you have symptoms that could be related to PFD and ask your doctor to refer you to a Physical Therapist that specializes in the treatment of PFD.

























As the article mentions, PFD is a common condition that goes undiagnosed as most people are embarrassed by their issues. Fortunately, most do not realize that this their issues are usually treatable when confronted with medication and physical therapy sessions.
Physical therapists can help patients with common issues of pelvic floor dysfunctions which are bulked into categories of stress incontinence, urge incontinence or a mix of both. Stress incontinence is an involuntary leakage associated with increased intra-abdominal pressure. Urge incontinence is an involuntary leakage associated with sudden desire to void. These conditions could be a result of: lumbar or pelvis malalignment, postural abnormalities, childbirth trauma, surgical trauma, sexual abuse, pelvic inflammation or infection, hemorrhoids/fistula/fissure, bowel/bladder disorders, obesity, smoking, a chronic cough/asthma, repetitive lifting and straining/high impact exercise, nerve compression, or other neurological disorders.
As mentioned in the article, treatments include strength training with pelvic friendly tools (such as weighted cones), relaxation therapies, electrical stimulation in order to promote neurological re-education, as well as manual soft tissue treatment. It is always best to be proactive and perform pelvic floor exercises to prevent this condition from occurring, such as kegels exercises, core involvement exercises, and hip adduction exercises.